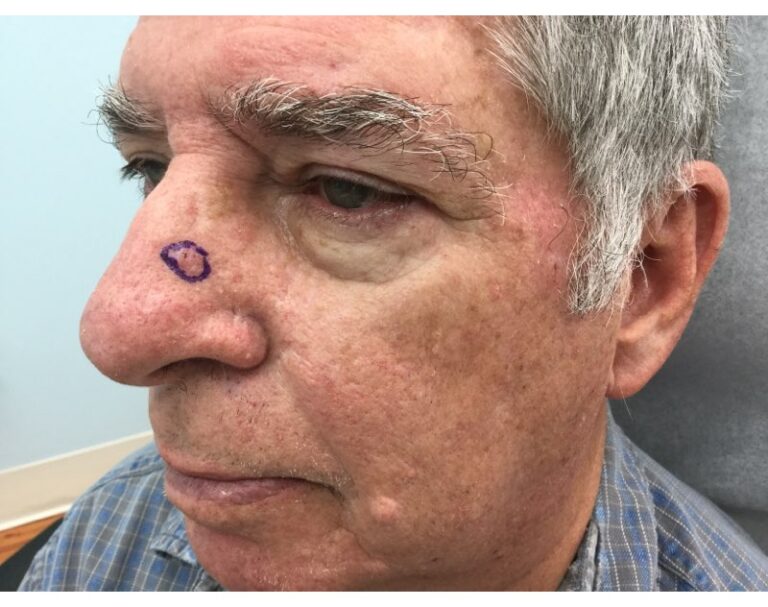
What does keratoacanthoma look like? It’s a raised skin tumor that appears in a dome-like shape. While it may closely resemble a pimple, it is actually more serious as it could be a precursor to cancer. Can keratoacanthoma spread, and is it malignant? We’re exploring these answers as well as keratoacanthoma symptoms and treatment in this overview.
Who Gets Keratoacanthoma?
It’s rare for people under the age of 20 to have keratoacanthoma. Generally, it affects people with fair skin who are 60 and over. Men are twice as likely to have keratoacanthoma than women. While the cause of keratoacanthoma isn’t exactly clear to doctors, there are some risk factors that can increase a person’s likelihood of developing one or more of these tumors:
- Exposure to UV rays
- HPV infection
- Some cancer-causing chemicals
- Genetics
- A weakened immune system
Is a Keratoacanthoma Malignant?
Keratoacanthoma is identified as an almost volcano-shaped lesion with a slight depression at its center that contains dead skin cells. It’s typically red in color and small to start, but can grow rapidly, doubling in size over the course of months. Keratoacanthoma may begin in a hair follicle and appear anywhere that sees excessive sun exposure, including the:
- Head
- Face
- Neck
- Hands
Keratoacanthoma is considered a metaplasia or premalignant condition, meaning that it has not yet developed into cancer but has the potential to do so. Due to the quick growth of this particular skin tumor, its makeup can change dramatically in a short period of time. It can go away on its own, but for some patients, a keratoacanthoma lesion can develop into squamous cell skin cancer, which is the second most common type of skin cancer.
Can Keratoacanthoma Spread?
Yes, keratoacanthoma can spread if left undetected or untreated. While the original tumor may shrink and disappear, it’s not uncommon for another to develop down the line, opening the opportunity for it to spread to other parts of the body.
One of the bigger differences between squamous and basal cell skin cancers is that squamous cell carcinoma is much more likely to spread. Even though keratoacanthoma is not cancer, it’s best to have these lesions removed as soon as they are found to limit risk.
How is Keratoacanthoma Diagnosed?
If your doctor suspects that you have keratoacanthoma, they may first complete a dermoscopy to assess the size and depth of the area. If the area seems too much like squamous cell skin cancer, your dermatologist may recommend an excisional biopsy. This is considered a complete treatment (as long as no part of the tissue is left behind), because it involves cutting through the skin to completely remove the area, so it can be examined under a microscope.
Squamous Cell and Keratoacanthoma Treatment
Should you be diagnosed with either keratoacanthoma or squamous cell skin cancer, treatment options range between various levels of surgery and radiation. It depends on your individual situation. If you have multiple keratoacanthomas, your dermatologist may suggest radiotherapy to avoid making multiple cuts.
Image-Guided Superficial Radiotherapy, or Image-Guided SRT, is the least invasive keratoacanthoma and squamous cell skin cancer treatment, as it effectively destroys the diseased cells without cutting or surgical scarring. Your symptoms will help determine which treatment method will be most effective for you.
Treat Squamous Cell Skin Cancer with GentleCure
To learn more about how Image-Guided SRT works and whether it’s right for your common skin cancer diagnosis, call our skin cancer information specialists at 855-936-4411. We’re here to answer your questions and give you the information you need to make an informed decision.